 Welcome to FMF LOVED. Unlock a world of medical education.
Welcome to FMF LOVED. Unlock a world of medical education.
FMF LOVED shares the best of FMF—curated and recorded sessions from our renowned in-person event. Dive into a treasure trove of medical knowledge, expert insights, and groundbreaking discussions, all available at your fingertips! Embrace the future of medical learning with FMF LOVED. Whether you’re a seasoned FMF attendee or considering FMF for the first time, this is your chance to access the excellence of FMF from anywhere in the world.
Available from February 14, 2024, to August 31 ,2024. You must complete a post-reflective survey for each session and your credits will be uploaded directly into your account in September 2024. This one-credit-per-hour Self-Learning program has been certified by the College of Family Physicians of Canada (CFPC) for up to 36 Mainpro+ credits.
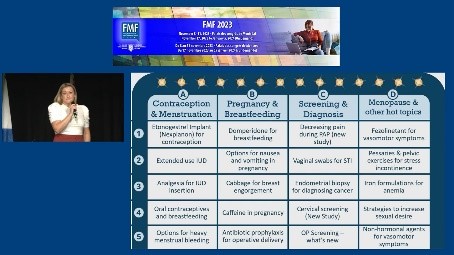
Jessica Kirkwood, MD, CCFP (AM); Danielle Perry, MSc RN; Samantha Moe, PharmD, ACPR
AFABulous Review: PEER presents an ode to women’s health
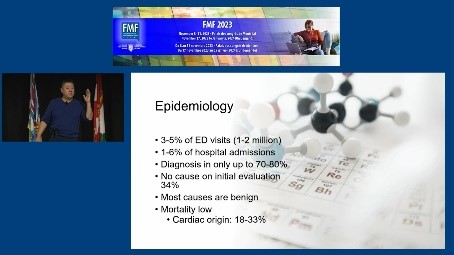
Vu Kiet Tran, MD, FCFP (EM),
MHSc, MBA, ICD.D
An Efficient Approach to Assessing Syncope
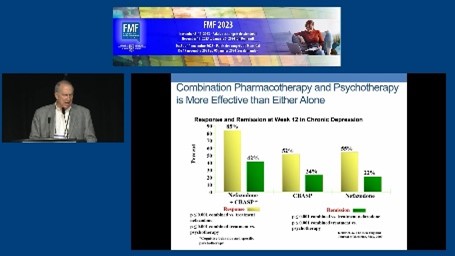
Jon Davine, MD, FCFP, FRCP(C)
Approach to Depression in Primary Care
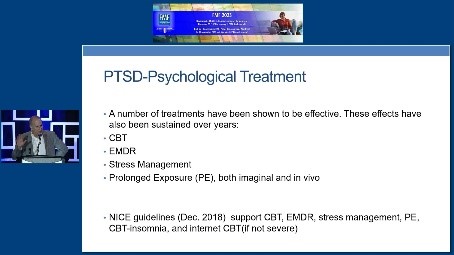
Jon Davine, MD, FCFP, FRCP(C)
Approach to PTSD in Primary Care
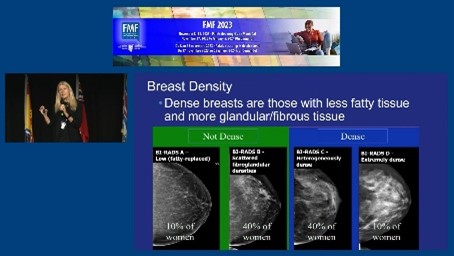
Anna Wilkinson, MSc, MD, CCFP, FCFP; Jean Seely, MD, FRCPC
Beyond the Basics of Breast Screening: What to do for young, old, dense and high-risk
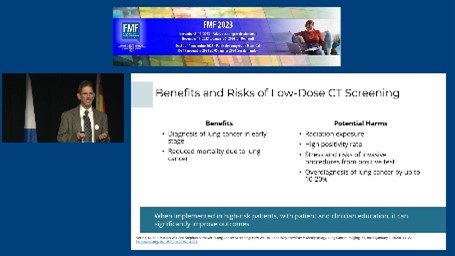
Alan Kaplan, CCFP, EM, FCFP
Cancer Screening Highlighting on Lung Cancer Screening

Michael Kolber, MD, CCFP, MSc; Adrienne Lindblad, BSP, ACPR, PharmD; Samantha Moe, PharmD, ACPR
Choose Your Briefs: Audience-selected clinical topics from PEER’s game board

Tara Kiran, MD, MSc, CCFP, FCFP ; Elly Grabner
Co-Designing The Future of Primary Care With Patients and The Public

Ted Jablonski, MD, CCFP, FCFP
Dispelling the Myths of the Petulant Prostate
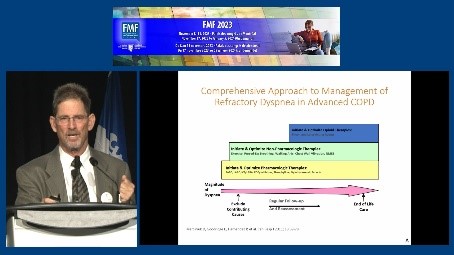
Alan Kaplan, CCFP (EM), FCFP
Dyspnea: How to assess and manage in the office

Lawrence Leung, MBBChir, DipPractDerm, FRCGP, FRACGP, FCFP
Eczema? Psoriasis? Or else?
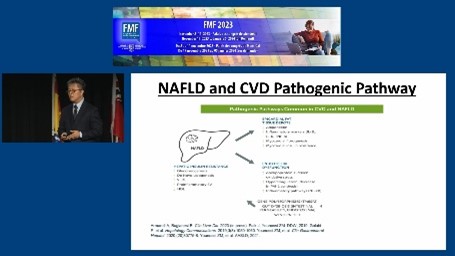
James Kim, MBBCh, PgDip; Akshay Jainn, MD, FRCPC, FACE, CCD, ECNU, DABIM, DABOM
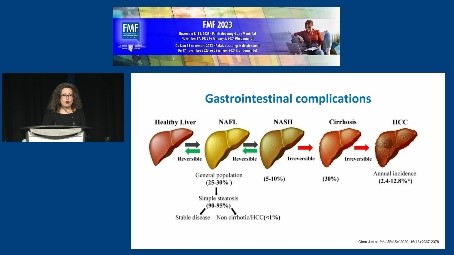
Hidden Complication of Diabetes and Obesity: Non-alcoholic fatty liver disease
Gord Arbess, MD, CCFP; James Owen, MD, CCFP
HIV 2023: PreP/PEP and other pearls
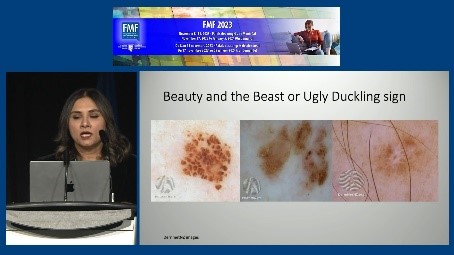
Saadia Jan, MBBS, FCFP, MClSc, DipPDerm(UK); Lynn Fong, MD, CCFP, DipPDerm(UK)
I Spy With My Little Dermatoscope
Kannin Osei-Tutu, MD, CCFP, FCFP
Igniting Change: Centering shared humanity and inclusive compassion – Towards greater social justice in medicine
Erin Gallagher, MD, CCFP (PC), MPH
Incorporating a Palliative Approach Into Your Family Practice
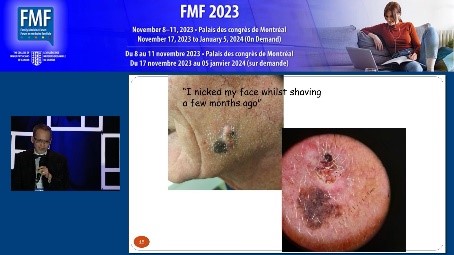
Lawrence Leung, MBBChir, DipPractDerm, FRCGP, FRACGP, FCFP; Horace Yu, MD, CCFP (EM)
Is This Skin Cancer?
Allan Grill, MD, CCFP (COE), MPH, FCFP
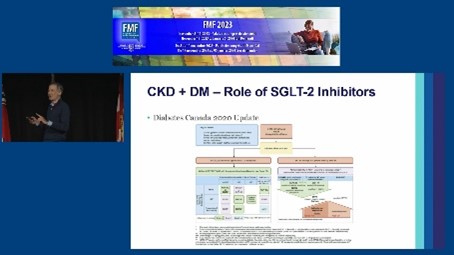
KidneyWise Update: Primary care essentials for managing CKD
Nick Kates, MBBS, FRCPC, MCFPC (hon)
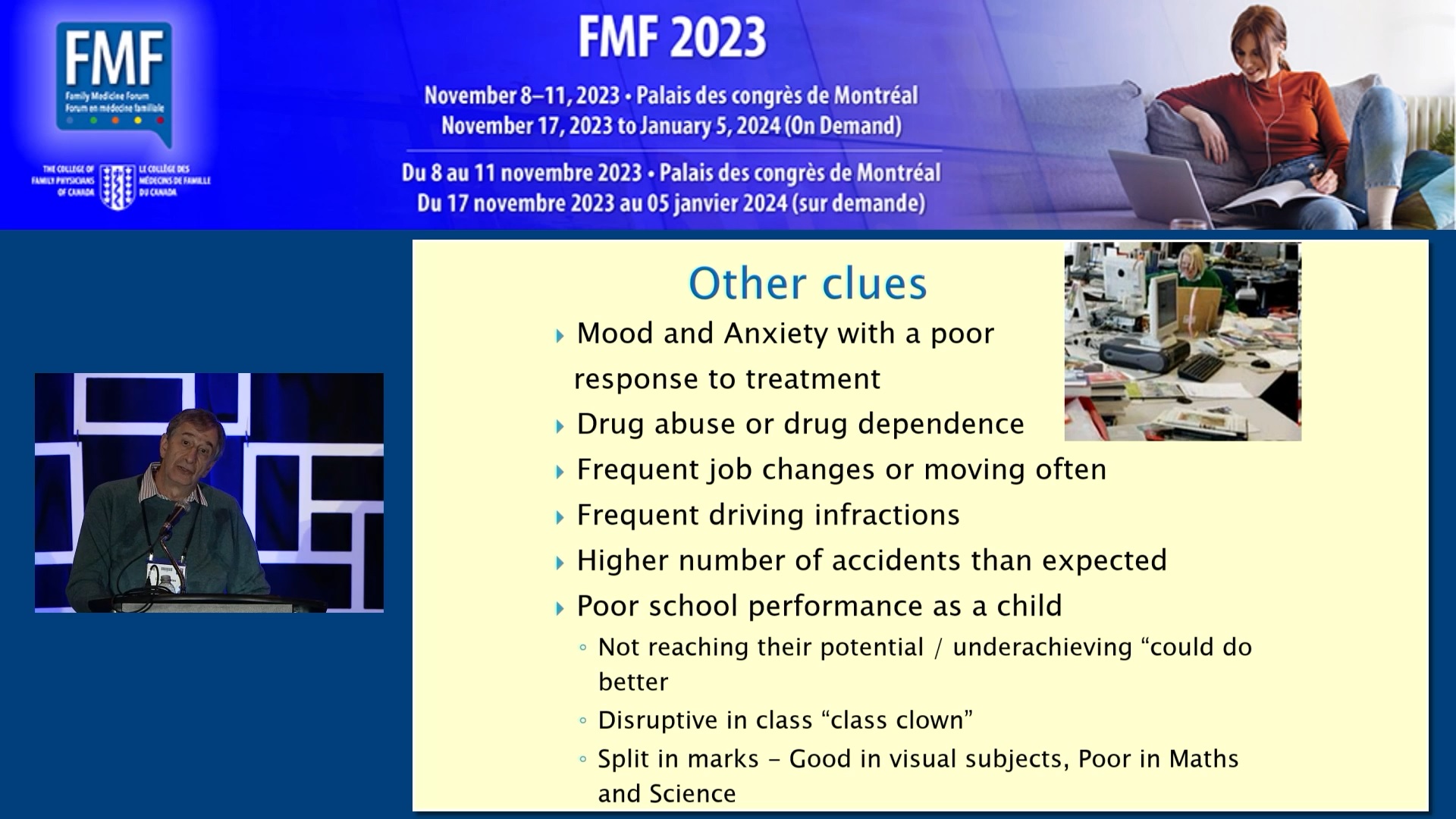
Managing ADHD in Adults in Your Practice
Douglas Green, MD, FRCP (Psychiatry)
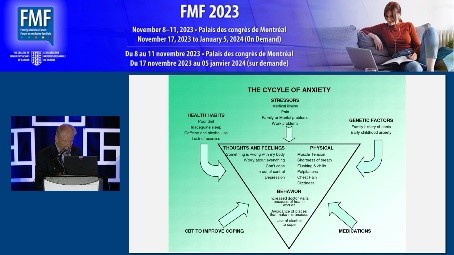
Managing Anxiety Conditions With the Ottawa Anxiety Algorithm
Nick Kates, MBBS, FRCPC, MCFPC (hon)
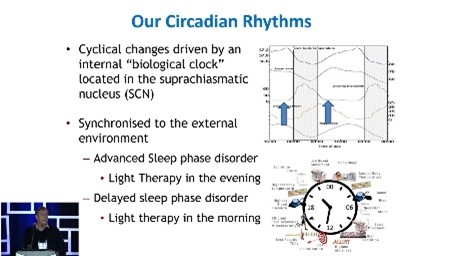
Managing Insomnia in Your Practice
Moshe Ben-Shoshan, MD, MSc; Jennifer Gerdts, Bcomm
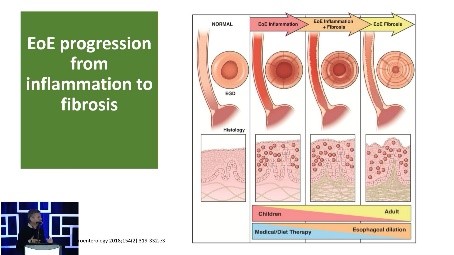
Navigating Non-IgE-Mediated Food Allergy

Jennifer Young, MD, CCFP (EM); Emelie Braschi, MD, CCFP; Jessica Kirkwood, MD, CCFP (AM)
PEER in the Clinic: Putting evidence into audience-selected cases
Tina Korownyk, MD, CCFP; Michael Allan, MD, CCFP; Danielle Perry, MSc RN
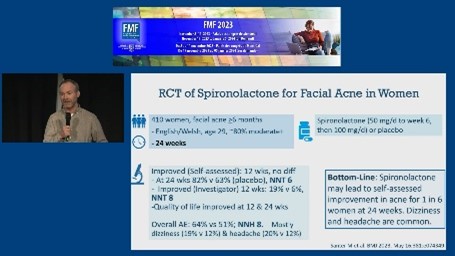
PEER: What’s new, what’s true and what’s poo?
Pierre-Paul Tellier, MD, CCFP, FCFP; Mélanie Henderson, MD, FRCPC, PhD
Preparing for the New Canadian Pediatric Obesity CPG: What you need to know
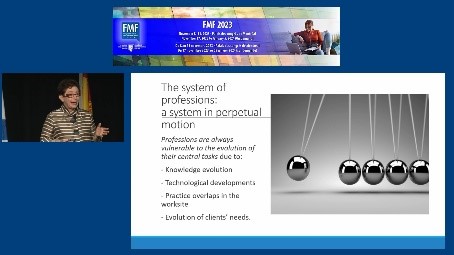
Marie-Dominique Beaulieu,C.M., C.Q., M.D., M.Sc., FCMF
Proud to Be Who We Are: Generalists!

Kathy Do, MD, MSc, CCFP
Psychedelic Assisted Therapy: A primer for family physicians
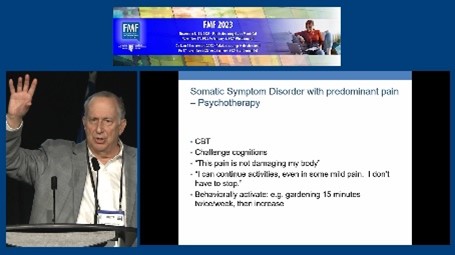
Jon Davine, MD, FCFP, FRCP(C)
Somatizing: What every family physician needs to know

Allison Paige, MD, CCFP
Tackling Barriers to Access in Primary Care
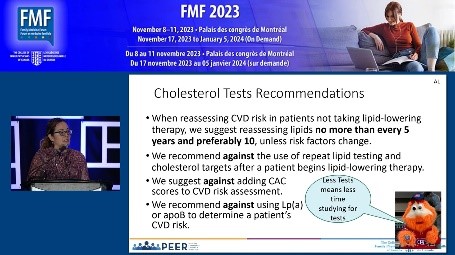
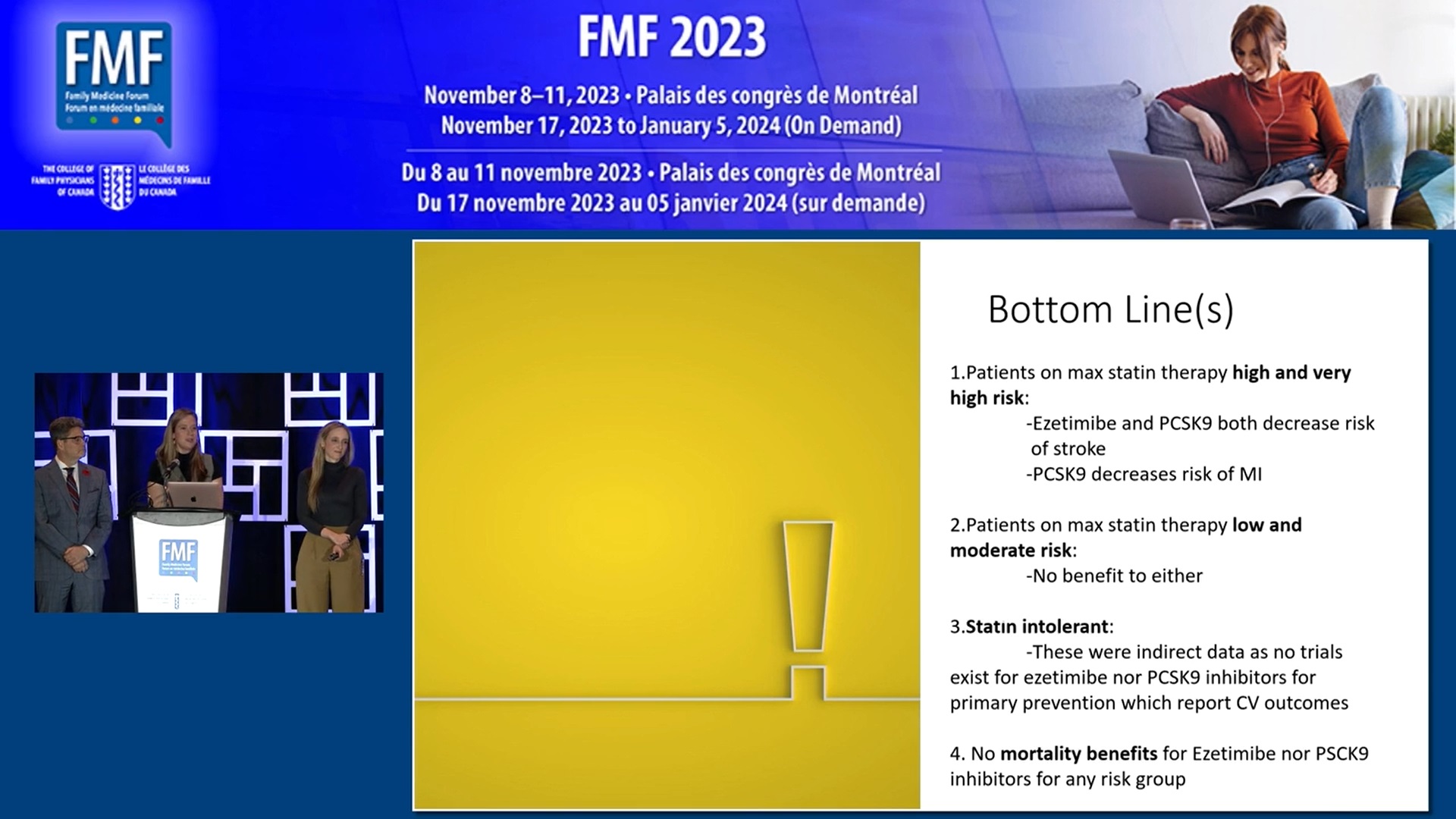
Adrienne Lindblad, BSP, ACPR, PharmD; Nicolas Dugré, PharmD, MSc; Michael Kolber, MD, CCFP, MSc
The 2023 PEER Simplified Lipid Guideline
Ted Jablonski, MD, CCFP, FCFP
The Push and Pull of Sex in Cancer Survivors: What can we learn?

Anna Wilkinson, MSc, MD, CCFP, FCFP
Tips and Tricks to Expedite Cancer Diagnosis
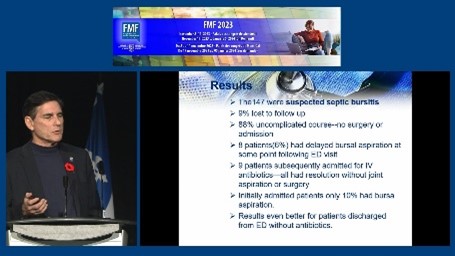
Jock Murray, MD, CCFP (EM); Constance Leblanc, MD, MSc., FCCP, CCFP (EM); Ryan Hennebery, MD, CCFP (EM); Mike Clory, MD, CCFP (EM); Matt Clarke, MD, CCFP (EM)
Top 10 Emergency Articles That Could Change Your Practice
Jock Murray, MD, CCFP (EM); Mandi Irwin, MD, CCFP; Jennifer Leverman, MD, CCFP (EM)
Top 10 Family Medicine Articles That Could Change Your Practice
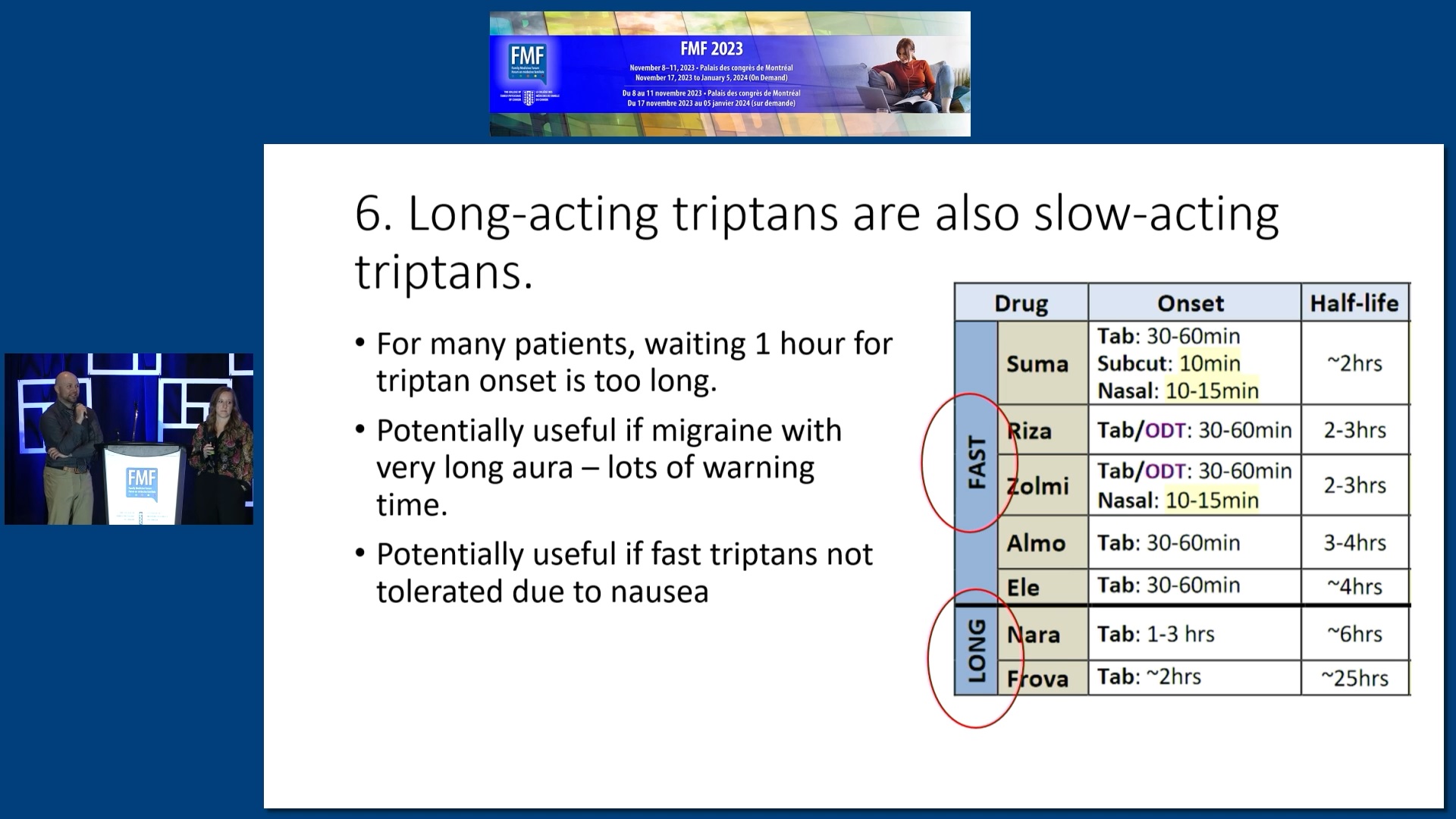
Alex Crawley, BSP, ACPR; Jackie Myers
Top 15 Pearls for Helping Your Migraine Patients

Kassandra Briand, MD
Transitioning to Practice 101
